In the complex world of healthcare in the USA, medical billing plays a crucial role in connecting providers, insurance companies, and patients to ensure smooth financial transactions. Yet, one of the biggest challenges healthcare providers face today is patient payment collection — an issue that can significantly impact cash flow, operational efficiency, and patient satisfaction.
The healthcare billing landscape is evolving rapidly with rising patient financial responsibility, insurance complexities, and regulatory demands. Successfully solving these patient payment challenges requires more than just traditional billing; it demands an integrated approach combining technology, best practices, and clear communication.
In this blog, we’ll explore the core difficulties of patient payment collection and reveal how effective medical billing strategies can help healthcare organizations streamline revenue cycles, reduce denials, and improve payment collections.
Table of Contents
ToggleUnderstanding Medical Billing and Patient Payment Collection
First, it’s essential to clarify what is medical billing and why it is so vital. Medical billing is the administrative process where healthcare services are translated into billing claims submitted to insurance companies or patients for payment. It’s the financial backbone of healthcare, ensuring providers receive reimbursement for services delivered.
Medical billing encompasses multiple tasks — from verifying insurance coverage to submitting claims, tracking denials, posting payments, and communicating with patients about their balances. When done right, billing in healthcare ensures transparency and timeliness, crucial to maintaining a healthy revenue cycle.
One critical aspect is how patient payment fits into this process. With healthcare costs rising, patients often bear a larger share of medical bills via copays, coinsurance, or deductibles. Collecting these payments promptly is key, but many healthcare providers find this particularly challenging, leading to increased accounts receivable and financial strain.
Common Challenges in Patient Payment Collection
Despite the essential nature of healthcare billing, providers face several obstacles that complicate patient payment collection:
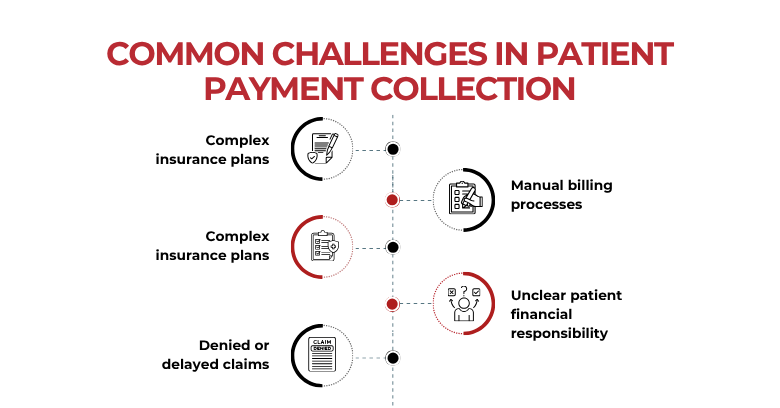
- Complex insurance plans — Different insurance policies come with varying coverage rules, making eligibility verification and billing tricky. Patients often do not understand their benefits fully, causing confusion about what they owe.
- Lack of patient engagement — Patients frequently receive bills after care with little explanation, which can lead to delayed payments or disputes.
- Denied or delayed claims — Errors in documentation, coding, or missing information can cause insurance claims to be denied or delayed, prolonging the payment process.
- Manual billing processes — Many organizations still rely on manual or semi-automated workflows that increase the risk of errors, missed deadlines, and inefficiencies.
- Unclear patient financial responsibility — Without upfront discussions about payment expectations, patients are surprised by bills, resulting in dissatisfaction and lower collection rates.
These challenges not only hurt provider cash flow but also increase administrative costs and reduce time available for quality patient care.
| You’ve learned about the importance of effective medical billing and the challenges that come with patient payment collections. If you’re looking to streamline your revenue cycle and improve payment collections, why not let experts handle it for you? Discover how our tailored medical billing solutions can help your practice overcome billing challenges and improve cash flow. Contact Geeks of Kolachi today to learn more! |
The Role of Technology in Medical and Billing Efficiency
Technology is a game-changer in overcoming many patient payment challenges. Advanced software and automation have transformed billing medical services from a labor-intensive process into an efficient, accurate operation.
Here’s how technology makes a difference:
- Electronic Health Records (EHR) integration: Seamless linking of patient clinical data with billing information ensures charges are accurately captured and coded.
- Practice Management Systems (PMS): These platforms automate appointment scheduling, insurance verification, claims submission, and patient billing in one place.
- Claim Scrubbing Software: Before claims are submitted, scrubbing tools check for missing or incorrect codes, reducing denials.
- Clearinghouses: Acting as intermediaries, clearinghouses format and verify claims according to payer requirements, speeding up reimbursement.
- Online patient portals: These portals allow patients to view bills, check balances, and make payments conveniently, increasing payment timeliness.
These digital solutions reduce human error, speed up claim processing, and improve the patient’s billing experience — all critical to enhancing medical and billing efficiency.
For in-depth resources on billing practices and tools, you can check the American Academy of Professional Coders (AAPC).
For organizations looking to leverage technology to optimize their billing processes, exploring healthcare software solutions can provide tailored tools for managing complex billing workflows.
Best Practices for Effective Medical Billings
Technology alone isn’t enough. To truly solve patient payment challenges, healthcare providers should adopt a holistic approach combining operational best practices of billing and medical:
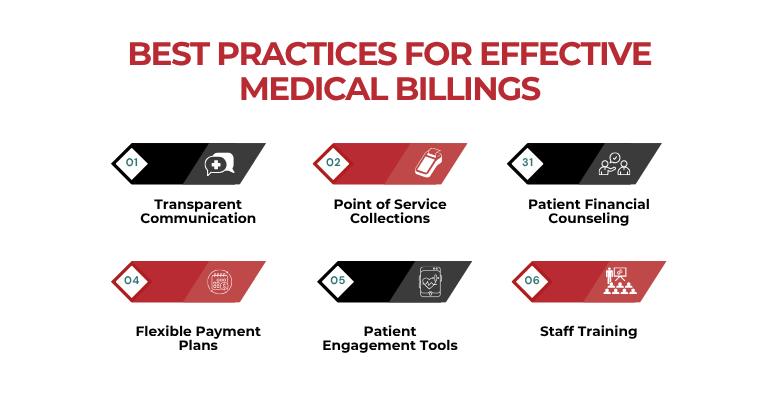
- Transparent Communication: Inform patients about their insurance coverage, copays, and out-of-pocket costs before or during their visit. Clear information reduces surprises and builds trust.
- Point of Service Collections: Collect payments like copays and deductibles during check-in or checkout to reduce outstanding balances later.
- Patient Financial Counseling: Offer dedicated staff or resources to help patients understand their bills and payment options.
- Flexible Payment Plans: Many patients struggle to pay large bills upfront. Offering installment plans or financing can increase collection rates and reduce bad debt.
- Patient Engagement Tools: Use reminders via email, text, or phone to notify patients about upcoming payments or outstanding balances.
- Staff Training: Equip biller medical teams with the skills to handle denials, appeals, and patient queries efficiently.
- Streamlined Denial Management: Quickly identify and address denied claims, correcting errors or appealing when appropriate, to avoid revenue loss.
By integrating these strategies with technology, healthcare providers can optimize billing for medical services and reduce revenue cycle friction.
For additional information on coding and billing standards, you can refer to the Medical Group Management Association (MGMA) website.
For additional information on bespoke software development that meets the unique needs of healthcare organizations, visit our service page for tailored solutions.
Compliance and Data Security in Medical Billing
Handling sensitive medical billing information requires strict adherence to privacy and security regulations such as HIPAA. Protecting patient data is paramount in maintaining trust and avoiding costly penalties.
Healthcare providers must implement:
- Secure data storage and transmission systems
- Access controls and employee training on data privacy
- Compliance checks to ensure billing systems meet legal standards
In medical insurance billing, where confidential patient and financial data frequently pass between parties, maintaining robust cybersecurity measures protects both patients and providers.
For further details about medical billing compliance and related regulations, refer to the Centers for Medicare & Medicaid Services (CMS) website.
Learn more about the importance of healthcare cybersecurity and its impact on patient data protection and clinical outcomes by reading our related blog post.
How Outsourcing Medical Billing Services Can Help
For many healthcare providers, partnering with professional medical billing services offers significant advantages in tackling patient payment challenges. Outsourcing billing allows providers to:
- Leverage specialized expertise in coding, claim management, and payer rules
- Utilize advanced technology without heavy upfront investments
- Improve claim accuracy and reduce denials with dedicated resources
- Enhance patient payment collection through focused follow-up and financial counseling
By shifting billing responsibilities to experts of medical billing services, healthcare organizations can focus on patient care while enjoying improved cash flow and reduced administrative burden.
Healthcare providers seeking to streamline their billing processes may benefit from solutions offered by organizations like the Healthcare Financial Management Association (HFMA), which provides resources for revenue cycle improvement.
Conclusion
Navigating the challenges of patient payment collection requires a well-rounded approach that combines modern technology, clear communication, compliance, and skilled billing staff. Optimizing medical billing in USA through automation, best practices, and possibly outsourcing ensures faster reimbursements, reduced denials, and higher patient satisfaction.
At Geeks of Kolachi, we understand the critical role of efficient health care billing and offer tailored billing services medical solutions designed to boost your revenue cycle performance and patient engagement.
| We know medical billing can be complex and time-consuming. If you’re ready to take the stress out of billing and improve your practice’s revenue cycle, we’re here to help! Get in touch with our team at Geeks of Kolachi and let’s make billing simpler and more efficient for you. Click here to schedule a free consultation! |
Frequently Asked Questions
What is medical billing?
Medical billing is the process of submitting and following up on claims with health insurance companies to receive payment for services provided by healthcare professionals.
How does medical billing work?
After receiving treatment, the provider submits a claim to the insurance company. The insurer processes the claim, and the provider bills the patient for any remaining balance.
What is an Explanation of Benefits (EOB)?
An EOB is a statement from your insurance company detailing what treatments and services were covered, how much they paid, and what you may owe.
Why was my medical bill so high?
High bills can result from factors like out-of-network care, high deductibles, or uncovered services. Review your EOB and discuss with your provider for clarification.
How can I dispute a medical bill?
Contact your provider’s billing department to discuss discrepancies. If unresolved, file a formal appeal with your insurance company.
What are CPT and ICD codes?
CPT codes describe medical procedures, while ICD codes identify diagnoses. Both are used for billing and insurance purposes.
How can I avoid medical billing errors?
Verify insurance details before treatment, request itemized bills, and promptly address any discrepancies with your provider.
How can I set up a payment plan for medical bills?
Contact your provider’s billing department to discuss payment options. Many offer flexible plans to accommodate financial situations.
What should I do if my insurance claim is denied?
Review the denial notice, correct any errors, and resubmit the claim. If necessary, appeal the decision with supporting documentation.
What is the difference between medical billing and coding?
Medical billing involves submitting claims for payment, while coding assigns standardized codes to diagnoses and procedures for billing purposes.