In recent years, telemedicine has transformed from a niche offering into a mainstream solution, significantly altering the way healthcare is delivered. What was once considered a convenience for some has now become an essential component of modern healthcare. This shift gained substantial momentum in the wake of the COVID-19 pandemic, which catalyzed the adoption of digital health solutions across the globe. The ability to access care from home has become a lifeline for many patients, and as digital transformation continues, telemedicine services are reshaping the healthcare landscape.
However, as healthcare technology continues to evolve, it’s important to weigh the pros and cons of telemedicine before making a decision about its integration into healthcare practices. From virtual consultations to remote patient monitoring, telemedicine is becoming more accessible and appealing to both patients and providers alike. In this blog, we will explore whether investing in telemedicine apps and software is truly worth it by examining the advantages and the challenges associated with its use in 2025.
Table of Contents
ToggleWhat is Telemedicine?
To understand the pros and cons of telemedicine, we first need to define what telemedicine entails. Telemedicine refers to the remote delivery of healthcare services through technology, including video consultations, telephonic interactions, and remote monitoring. Patients and healthcare providers can connect in real-time from anywhere, whether they are across town or in different regions. This interaction is facilitated by smartphones, computers, and specialized telemedicine software.
What is Telehealth?
While telemedicine focuses on clinical services, telehealth is a broader concept that extends beyond medical consultations. So if you’re thinking how does telehealth work? telehealth basically encompasses the use of technology to deliver a wide range of healthcare services and information. It includes virtual consultations, but also involves the remote monitoring of health conditions, the sharing of medical data, and even the training of healthcare professionals through digital platforms. Essentially, telehealth integrates telemedicine within a broader framework of health-related services, such as wellness programs and health education.
Harvard Health provides an in-depth look at the advantages and disadvantages of telehealth, which can help you better understand its role in modern healthcare.
In addition to traditional care, telehealth also facilitates ongoing communication between healthcare providers and patients, improving engagement and patient empowerment. Benefits of telehealth include making healthcare more accessible, especially for individuals in remote or underserved areas who may otherwise struggle to receive care. As digital tools continue to improve, telehealth is playing an increasingly important role in enhancing the efficiency of healthcare delivery and broadening access to care for individuals who need it most.
| Worried about data breaches or insecure medical systems slowing down your patient care? Let’s change that. Talk to our healthcare cybersecurity experts and discover how to keep your clinical data safe without disrupting your workflow. Schedule a Free Consultation Today. |
The Pros of Telemedicine
Although telemedicine might not be suited for every healthcare situation, it provides several advantages that have made it a popular choice among both healthcare providers and patients. Here are some of the most significant benefits of telemedicine.
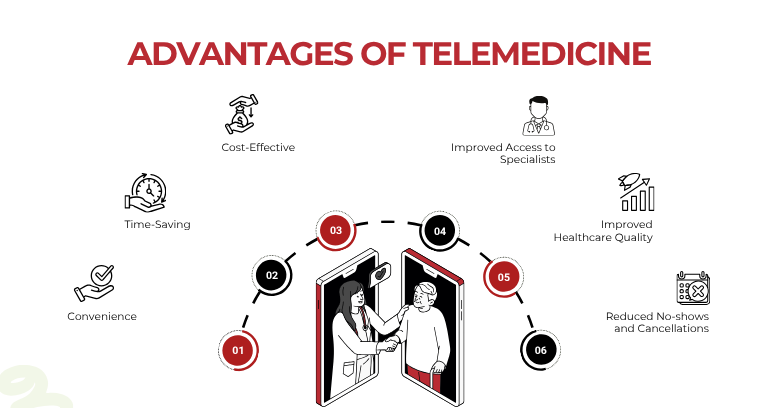
1. Convenience
The most immediate benefit of telemedicine is its convenience. For patients, traditional healthcare visits often involve leaving home, waiting in long lines, and spending time in transit. With telemedicine apps and telemedicine software, these hurdles are eliminated. Patients can now receive care from the comfort of their own homes, significantly reducing the time and effort spent on healthcare appointments.
For those living in remote areas, telemedicine offers a critical lifeline. Rural and underserved populations often have limited access to healthcare facilities, making it difficult for them to receive proper care. By enabling remote consultations, telemedicine ensures that these individuals can access healthcare without the need to travel long distances.
Healthcare providers also benefit from this convenience. Telemedicine allows them to treat patients remotely, regardless of location. By reducing the geographic limitations on patient care, providers can reach a larger patient base and improve service delivery. Explore how you can integrate healthcare software solutions to optimize your telemedicine services.
A comprehensive overview of Medicare’s telehealth coverage in 2025 can be found on the Kaiser Family Foundation’s website, clarifying what patients can expect in terms of reimbursement and coverage.
2. Time-Saving
Scheduling an in-person healthcare appointment often involves long waiting times, both for booking and during the visit itself. In many cases, patients may wait for weeks for a scheduled appointment, only to spend additional hours waiting in the doctor’s office. With telemedicine, these problems are minimized. Virtual consultations allow patients to meet with their healthcare providers at their scheduled times without the long wait.
For healthcare professionals, such telemedicine benefits streamline their day. By reducing patient wait times and travel-related delays, healthcare providers can schedule more appointments per day, making their workflow more efficient. This time-saving factor is especially crucial for primary care providers who need to manage a high volume of patients.
3. Cost-Effective
The high costs of healthcare continue to be a concern for many patients, especially those without adequate insurance. Telemedicine services can provide a more affordable alternative to in-person visits. Since telemedicine removes the need for travel, parking, and office overhead, the costs of virtual consultations are typically lower than traditional appointments.
For healthcare providers, adopting medical software reduces operational expenses as well. Providers can save on overhead costs such as renting office space, maintaining medical equipment, and staffing requirements. Additionally, telehealth benefits including helping in preventing expensive emergency room visits by enabling patients to consult with a healthcare provider remotely before deciding if a physical visit is necessary.
According to a report from the American Hospital Association, telehealth is expected to continue evolving in 2025, with new trends and insights emerging.
4. Improved Access to Specialists
One of the challenges patients face is accessing specialist care, particularly in rural or underserved areas where specialists may not be available. Telemedicine offers a solution by enabling patients to connect with healthcare specialists remotely. Whether a patient requires a consultation with a cardiologist, neurologist, or psychologist, telemedicine allows them to access expert care without traveling long distances.
This is especially significant for individuals with mobility limitations or chronic conditions that make traveling difficult. Through telemedicine services, they can easily consult with the specialists they need, regardless of their location.
For an up-to-date look at the top telehealth trends in 2025, Healthcare Transformers highlights the latest innovations shaping the future of healthcare.
5. Improved Healthcare Quality
Another significant advantage of telemedicine is its ability to improve healthcare outcomes. Through these medical apps, patients can track their symptoms and vital signs, providing real-time data to healthcare providers. This remote monitoring allows healthcare professionals to intervene early if any issues arise, preventing complications and improving patient outcomes.
For patients with chronic conditions like diabetes or hypertension, regular check-ins through telemedicine allow doctors to adjust treatment plans promptly. This continuity of care leads to better long-term management of these conditions.
In the field of telemental health, patients also report improved outcomes. Virtual consultations for mental health treatment have been shown to reduce levels of stress, anxiety, and depression, particularly for patients who otherwise might have had difficulty attending in-person sessions.
6. Reduced No-shows and Cancellations
Missed appointments are a common issue in healthcare. However, telemedicine can significantly reduce the rate of no-shows and cancellations. Since virtual visits are more convenient and require less effort for patients, they are more likely to attend their scheduled appointments.
Furthermore, telemedicine software can send reminders and follow-up notifications to patients, ensuring that appointments are not missed. This helps both patients and healthcare providers stay on track, ensuring that care is not delayed.
The Cons of Telemedicine
While the benefits of virtual care are considerable, there are also challenges that need to be addressed. Let’s examine some of the disadvantages that come with implementing telemedicine services in healthcare.
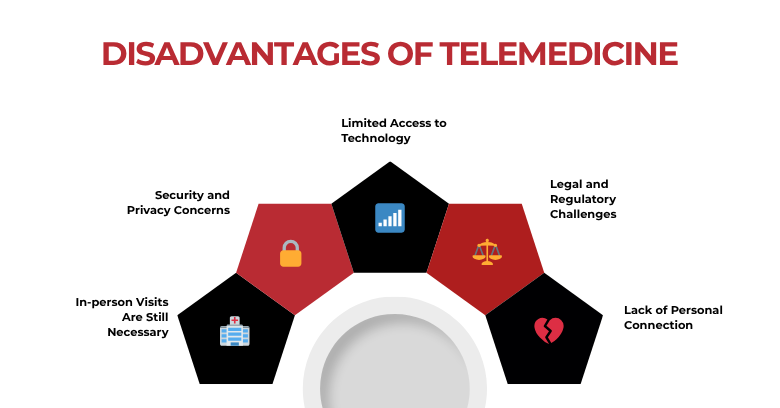
1. In-person Visits Are Still Necessary
Although telemedicine can address many types of consultations, it is not a replacement for all in-person visits. Certain diagnostic tests, such as blood work, imaging scans, and physical exams, cannot be performed remotely. In these cases, telemedicine serves as a supplement to, rather than a replacement for, traditional office visits.
Moreover, some health conditions may require a physical examination for accurate diagnosis and treatment. Without being able to directly examine a patient, healthcare professionals may miss crucial details, which could lead to misdiagnosis or an incomplete treatment plan.
2. Security and Privacy Concerns
Security remains one of the most significant problems with telehealth and telemedicine. Since healthcare providers are transmitting sensitive health information over the internet, there is a risk that personal data may be exposed to cyberattacks or breaches. Even though many telemedicine platforms are designed with encryption and comply with regulations like HIPAA (Health Insurance Portability and Accountability Act), no system is 100% secure.
Healthcare organizations must prioritize cybersecurity to ensure that patient data remains protected. They must also adhere to privacy regulations to maintain compliance and safeguard patient trust.
3. Limited Access to Technology
Although technology has rapidly advanced, not everyone has equal access to the devices or internet bandwidth required for telemedicine. For patients in rural areas or those with low incomes, the digital divide can limit access to healthcare. Many older adults and individuals with lower technological literacy may struggle to use telemedicine apps or may not have the necessary devices to participate in virtual consultations.
To ensure equitable access to healthcare, it’s essential for healthcare providers to address these technological barriers. This might include offering training on how to use telemedicine tools or providing patients with access to devices and internet connections.
4. Lack of Personal Connection
While medical apps offer virtual consultations, they cannot fully replicate the personal connection that comes with an in-person visit. Some patients may feel disconnected from their healthcare provider, especially if they are discussing sensitive or complex issues. This lack of face-to-face interaction can be particularly challenging in fields like telemental health, where building trust and rapport is crucial to successful treatment.
For some patients, the physical presence of a doctor is an important aspect of their care. The inability to shake hands, make direct eye contact, or feel the comfort of being in an office can make the consultation feel impersonal.
5. Legal and Regulatory Challenges
The regulatory landscape for telemedicine is complex and varies from state to state, as well as from country to country. Healthcare providers must navigate a variety of regulations to ensure they are compliant with local laws. For example, Medicare telemedicine 2025 policies differ from those of private insurance providers and Medicaid programs.
In some regions, state laws may limit healthcare providers’ ability to offer telemedicine across state lines, which could hinder the reach of their services. Additionally, healthcare providers must ensure that their malpractice insurance covers telehealth services, as many policies were originally designed with in-person visits in mind.
Is Telemedicine Worth the Investment?
Given the pros and cons of telehealth, the decision to invest in telemedicine depends on a variety of factors, including the specific needs of healthcare providers and patients. For healthcare organizations, telemedicine services can lead to cost savings, improved patient care, and increased access to patients. However, it’s essential to evaluate whether the technology fits within the practice’s infrastructure and patient base.
For patients, telemedicine offers an affordable and convenient alternative to traditional care, particularly for those with limited access to in-person services. However, some patients may still prefer in-person consultations, especially when it comes to more complex health issues.
While telemedicine is not without its challenges, such as data security and technology access, its benefits are undeniable. As technology continues to advance, the use of telemedicine is only expected to grow, making it a worthy consideration for both healthcare providers and patients alike.
For a deeper dive into the current telemedicine landscape, you can explore the latest telemedicine statistics from Market.us, which provide valuable insights into usage and trends.
Conclusion:
In conclusion, telemedicine has proven to be a valuable tool in improving healthcare access, reducing costs, and enhancing patient care. Despite its challenges, such as the need for in-person visits in certain cases and concerns over data privacy, the benefits far outweigh the drawbacks. For healthcare providers looking to stay competitive and offer superior care, investing in telemedicine and healthcare services can be a strategic move.
As we continue to adapt to the digital age, telemedicine is poised to play an even greater role in healthcare delivery. By embracing this innovative technology, healthcare professionals can ensure they are meeting the evolving needs of their patients while navigating the future of healthcare with confidence.
Find out more about optimizing healthcare operations with software development.
Looking for insights on improving patient payment management? Explore our blog post on medical billing challenges.
To stay informed about the latest developments in telehealth, Dimins offers a detailed analysis of the state of telehealth in 2025, highlighting key changes and expectations.
As the telemedicine landscape changes, it’s important to be aware of upcoming policy changes. The Telehealth Resource Center outlines the telehealth policy cliff that is expected in October 2025, which could impact the industry’s growth.
| Still relying on outdated security measures for your healthcare systems? Don’t wait for a cyberattack to expose your data or halt critical treatments. Let Geeks of Kolachi help you secure your healthcare environment end-to-end—from EHRs to IoMT devices. Contact us now to protect what matters most—your patients. |
Frequently Asked Questions
What are the benefits of telemedicine for patients and providers?
Telemedicine offers numerous benefits for both patients and healthcare providers. For patients, it provides convenience by allowing consultations from home, saving time and travel expenses. It also improves access to care, especially for those in rural or underserved areas. For healthcare providers, telemedicine reduces overhead costs, enhances workflow efficiency, and expands their reach to a broader patient base.
How does telemedicine work?
Telemedicine works by connecting patients and healthcare providers remotely using digital platforms such as video calls, phone consultations, and messaging. Patients schedule an appointment through telemedicine apps or websites, and the consultation occurs in real-time. These services can include primary care visits, specialist consultations, mental health therapy, and chronic disease management.
What are the drawbacks of telemedicine?
While telemedicine offers significant advantages, it has its drawbacks. It cannot fully replace in-person visits, especially for procedures that require physical exams or diagnostic tests. There are also concerns over data privacy and security, as sensitive health information is transmitted online. Additionally, some patients may struggle with the technology or lack reliable internet access, limiting the effectiveness of telemedicine in certain areas.
Is telemedicine safe and secure?
Yes, telemedicine is safe when the appropriate security measures are in place. Most telemedicine platforms use encryption to ensure that patient data is protected during transmission. Providers also comply with HIPAA (Health Insurance Portability and Accountability Act) regulations to maintain patient confidentiality. However, patients should always ensure they are using trusted platforms to protect their personal health information.
What types of healthcare services can be provided through telemedicine?
Telemedicine can be used for a wide range of healthcare services, including primary care, specialist consultations (such as cardiology or dermatology), mental health services, chronic disease management, and even post-surgical follow-ups. It is particularly useful for ongoing care, providing patients with convenient access to healthcare without leaving their homes.
How does telemedicine affect healthcare costs?
Telemedicine can lower healthcare costs in several ways. It reduces the need for in-person visits, cutting down on travel, office overhead, and administrative expenses. Additionally, telemedicine helps reduce emergency room visits and hospital readmissions by providing timely care that prevents complications. For patients, it offers a more affordable option, especially for those without insurance or in rural areas.
Can telemedicine replace in-person visits entirely?
Telemedicine cannot completely replace in-person visits. Certain healthcare needs, such as physical exams, diagnostic tests, or surgeries, still require a visit to a healthcare facility. However, telemedicine serves as a valuable supplement for many non-emergency situations and ongoing care, such as routine check-ups, mental health counseling, and management of chronic conditions.
Is telemedicine effective for mental health services?
Yes, telemedicine is highly effective for mental health services. It provides a convenient and confidential way for patients to access therapy, counseling, and psychiatric support. Virtual consultations help reduce stigma and make it easier for people in remote areas to receive the mental health care they need. Research shows that telehealth for mental health is as effective as in-person therapy for many patients.
What are the privacy and security concerns with telemedicine?
The main privacy and security concern with telemedicine is the risk of data breaches. Since telemedicine involves the transmission of sensitive health information online, healthcare providers must use secure, encrypted platforms to protect patient data. Providers also need to comply with regulations like HIPAA to ensure patient privacy. To reduce risk, patients should use secure networks and avoid sharing personal information on untrusted platforms.
Is telemedicine covered by insurance?
Telemedicine coverage varies by insurance provider and policy. Many health insurance plans now cover telemedicine visits, particularly after the COVID-19 pandemic, which led to a surge in remote care. It’s essential to check with your insurer to confirm whether telemedicine consultations are covered under your plan, and if so, what services are included.